On World AIDS Day, Canada must lead the way in combating HIV-AIDS - The Conversation Indonesia
Dec. 1 marks World AIDS Day. As researchers focused on fighting the HIV-AIDS epidemic, we are increasingly concerned all the progress made in the fight against the virus is at risk.
In 1996, the first remarkable breakthrough against the HIV-AIDS epidemic came with the novel combination of drugs that became known as Highly Active Antiretroviral Therapy (HAART).
For the first time, HAART was able to stop viral replication and render the virus undetectable in blood and bodily fluids, and consequently promote immune reconstitution. This in turn would prevent an HIV infection from developing into AIDS, significantly reducing premature deaths.
Treatment as prevention
The next major breakthrough came in the early 2000s. Through close monitoring of the epidemic in British Columbia, our research documented that HIV infected individuals who have consistent viral suppression with HAART are virtually unable to transmit the infection. This led us to recommend initiating HAART immediately following HIV diagnosis to accelerate overall HIV/AIDS control.
We called the strategy Treatment as Prevention (TasP) to illustrate the fact that HAART simultaneously stops progression to AIDS, premature death and HIV transmission.
TasP was enthusiastically embraced by the Joint United Nations (UN) Programme on HIV/AIDS (UNAIDS), in 2010. However, it soon became apparent that the TasP strategy was too ill defined, and this open the door for it to be inconsistently deployed between regions.
In 2014, UNAIDS unveiled two sequential TasP-inspired targets to quantify the proportion of people living with HIV who need to be diagnosed, the proportion of diagnosed people who need to be on HAART, and the proportion of people on HAART who need to be virologically suppressed by 2020 and 2025. Viral suppression is defined by having less than 200 copies of HIV per milliliter of blood.

These targets were specifically designed so that by 2030 the world would see a 90 per cent decrease in AIDS mortality and new HIV infections, and meet the goal of ending the HIV-AIDS pandemic. In 2015, the UN formally endorsed the 90-90-90 by 2020 target. It endorsed our subsequent 95-95-95 by 2025 target in 2021.
However, a lack of leadership and resources have hampered progress towards the UN targets around the world. This has been exacerbated by the COVID-19 pandemic, which disrupted some medical services, decreased HIV testing, interrupted the provision of HAART and diverted funding.
Differing success rates across Canada
In 2020, the Public Health Agency of Canada (PHAC) released a much-awaited epidemiological HIV/AIDS update. The update came ahead of the International AIDS Conference held in Montréal in July 2022.
Unfortunately, the results were rather concerning. HIV cases in Canada have remained flat since the 1990s, but there is a marked contrast between British Columbia and the rest of the country. While B.C. saw a steady decline in cases between 1996 and 2020, the rest of Canada saw no further reduction in cases over the same period.
HIV cases peaked throughout Canada in the early 80s. But a decrease in high-risk sexual practices led to a substantial reduction in cases. After that, the course of the epidemics diverged.
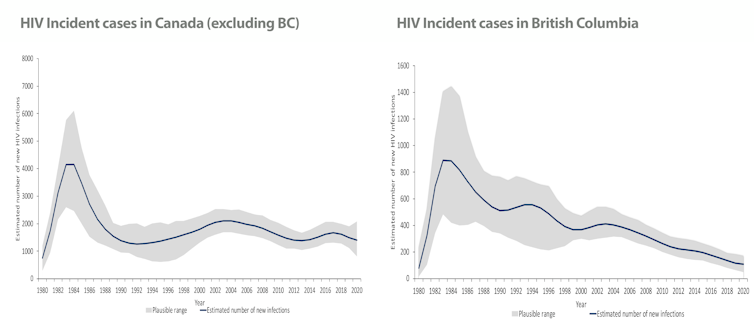
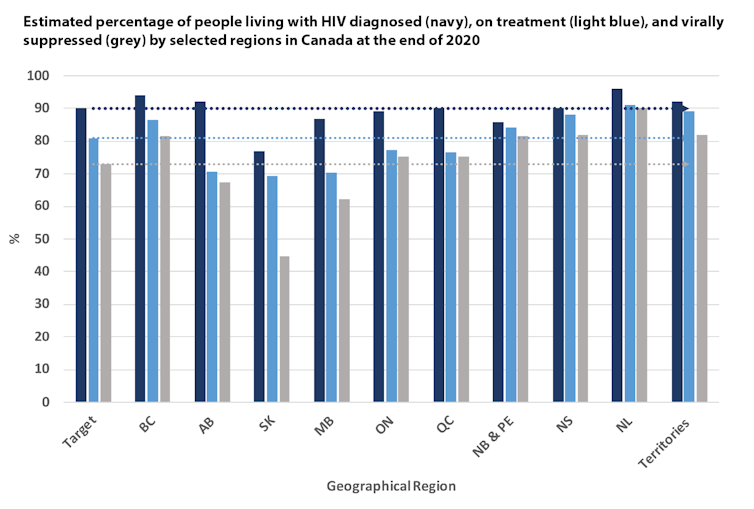
The reason for this discrepancy can be explained by the success of TasP in B.C., where the strategy originated. The graph below compares progress toward the UN's 2020 target across Canada's provinces and territories.
B.C., Nova Scotia, Newfoundland and Labrador and the three territories are the only Canadian jurisdictions that surpassed all three components of the benchmark target.
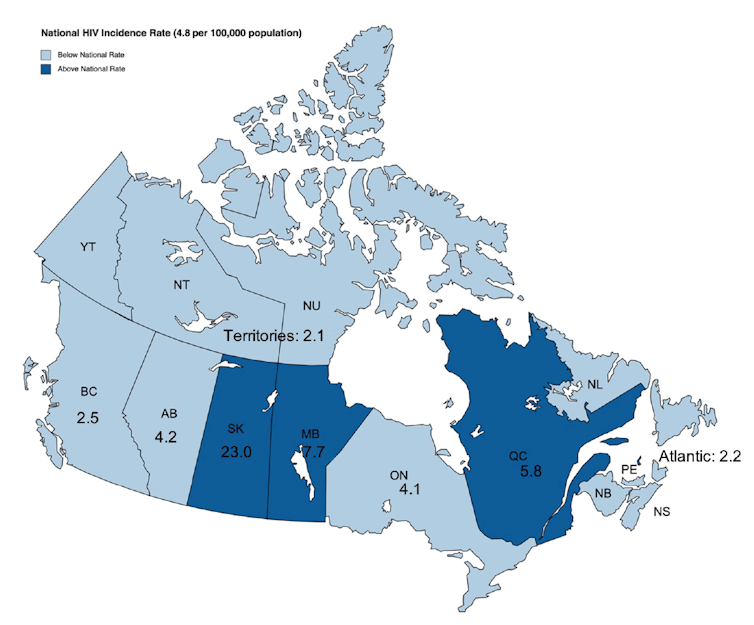
A failure to optimally implement TasP nationally has led to markedly different HIV rates across the country. In 2020, the national HIV incidence rate was 4.8 per 100,000 people. B.C., which had the highest domestic incidence rate at the peak of the epidemic in the 1980s, was well below the national average, at 2.5 per 100,000 population. The province is now at the low end of the national spectrum, together with the territories and Atlantic provinces at 2.1 and 2.2 per 100,000 population, respectively.
Alberta and Ontario were within the range of the national average at 4.2 and 4.1 per 100,000 population. At the other end, Saskatchewan, Manitoba and Québec were above the national average at 23.0, 7.7 and 5.8 per 100,000 population, respectively.
What Canada needs to do
Clearly, Canada has the tools and the means to end the epidemic. The question remains, are we up to the task? The key requirements are well known:
- Normalize HIV testing to ensure everybody knows their HIV status.
- Remove barriers to accessing health services.
- Expand support for affected populations, with particular emphasis on harder-to-reach and most affected populations (men who have sex with men, people dealing with substance use, sex workers, inmates, immigrants and First Nations Peoples).
- Make free harm reduction services widely available (condoms, lubricants, injection and smoking paraphernalia, supervised injection and smoking consumption sites and safer drug supply programs).
- Free HAART for all HIV-positive people.
- Free pre-exposure prophylaxis (PrEP) to all people at heightened HIV risk.
- Free relevant laboratory monitoring for all those on HAART or PrEP.
In addition, we must demand full transparency and accountability from our health-care system. That starts with PHAC annually reporting progress towards the UN 95-95-95 by 2025 target, HIV prevalence and AIDS-related mortality.
Finally, the federal government should sponsor a yearly independent summit of all relevant stakeholders to promote accountability and transparency, compare regional progress and share lessons learned in the process.
As a leader in treatment and prevention, Canada has a global responsibility to optimally implement a strategy to effectively combat HIV-AIDS. That will require a major commitment from the provinces given that health care is a provincial responsibility.
Canada knows how to end the HIV-AIDS epidemic. It is high time to get it done.
Comments
Post a Comment