Gonorrhea: Causes, Symptoms, Treatment & Prevention - Cleveland Clinic
Overview
What is gonorrhea?
Gonorrhea is a common sexually transmitted infection (STI) caused by a bacteria called Neisseria gonorrhoeae (N. gonorrhoeae). It's also sometimes called "the clap" or "drip." Gonorrhea is spread through sexual fluids, including vaginal fluid and semen. You can get gonorrhea from intercourse, anal sex, oral sex, or sharing sex toys with an infected person.
Often, gonorrhea doesn't cause symptoms. This makes it easy to infect your partners unknowingly. Getting tested frequently – according to your healthcare provider's recommendations – and safer sex practices can reduce your risk of infection.
Who gets gonorrhea?
Sexually active people of any age or sex can get gonorrhea and spread it to their partners. You can pass the infection on to your baby during childbirth.
You're at greater risk of infection if you:
- Are under 25.
- Have a history of STIs.
- Don't use condoms or dental dams each time you have sex.
- Are having sex with one or more partners who haven't tested negative for gonorrhea.
- Are a person with a penis who has sex with other people with penises (men who have sex with men/MSM).
How common is gonorrhea?
Gonorrhea is the second most common STI caused by bacteria – just behind chlamydia. Gonorrhea and chlamydia infections often happen together. Around 1.14 million new gonorrhea infections occur in the United States every year. About half of these infections occur in people ages 15 to 24.
Symptoms and Causes
What are the symptoms of gonorrhea?
Often, gonorrhea doesn't cause symptoms. This is especially the case in women and people assigned female at birth (AFAB). If you do experience symptoms, they'll likely impact you differently based on your reproductive parts.
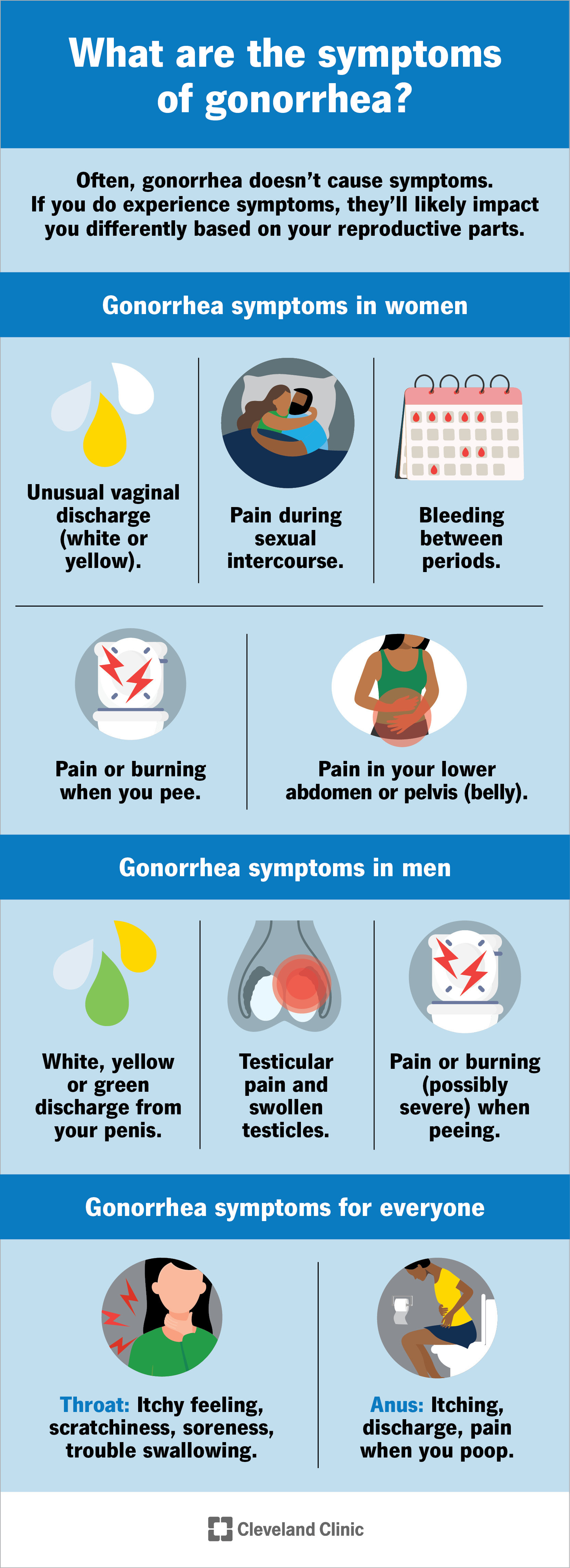
Gonorrhea symptoms vary depending on your reproductive anatomy.
Gonorrhea symptoms in women
People assigned female at birth – including cisgender women, transgender men and nonbinary people with vaginas – often don't experience symptoms. This is why it's essential to get tested for gonorrhea if you believe you've been exposed.
When symptoms are present, they may include:
Gonorrhea symptoms in men
People assigned male at birth – including cisgender men, transgender women and nonbinary people with penises – are more likely to experience symptoms. Still, you may not notice signs of infection until several weeks after you've been exposed, meaning that you can unknowingly infect partners.
Symptoms may include:
- White, yellow or green discharge from your penis.
- Pain or burning (possibly severe) when peeing (dysuria).
- Testicular pain and swollen testicles.
Gonorrhea symptoms in all genders
People of all genders can get gonorrhea infections in the throat (through oral sex on the genitals or anus) or rectum (through anal sex). These types of infections are less common than gonorrhea affecting the genitals.
Symptoms may include:
- Throat: Itchy feeling, scratchiness, soreness (similar to a sore throat), trouble swallowing.
- Anus: Itching, discharge, pain when you poop.
What causes gonorrhea?
You get an infection when the bacteria that causes gonorrhea (N. gonorrhoeae) enters your body through sexual fluids, like semen or vaginal fluid – often through unprotected sex. The bacteria can enter your body through a penis, vagina, mouth or anus. Neither you nor your partner has to ejaculate (cum) to spread the bacteria. You can also spread gonorrhea by sharing sex toys that haven't been washed or covered with a new condom.
In people assigned female at birth, the most common site of infection is the cervix. The cervix is the opening between your vagina and your uterus.
In people assigned male at birth, infection usually starts in the urethra, the tube where urine exits your body.
What doesn't cause gonorrhea?
Gonorrhea is contagious and spreads easily during sexual activity. Still, not all intimate acts or body fluid exchanges put you at risk for gonorrhea. You can't get gonorrhea from:
- Kissing, hugging or holding hands.
- Sharing food, drinks, or silverware.
- Using a toilet after someone else.
- Inhaling droplets after someone coughs or sneezes.
What causes gonorrhea in men?
You can get gonorrhea if you have sex with an infected person. This is the same, no matter your sex or gender. Vaginal intercourse, anal sex, oral sex and sharing sex toys that haven't been cleaned or protected with a condom can all expose you to the bacteria. Close genital to genital contact without penetration can expose you, too.
Diagnosis and Tests
How is gonorrhea diagnosed?
Your healthcare provider will ask you questions about your symptoms and sexual history. Then, your urine or body fluid will need to be tested for the bacteria that causes gonorrhea.
During your appointment, your provider may:
- Perform a pelvic exam, taking a fluid sample from your cervix for testing.
- Take a sample of fluid from your penis for testing.
- Swab your throat or rectum to collect fluid for testing.
- Take a urine sample for testing.
Your provider will discuss which type of gonorrhea test is best in your situation and what kind of fluid sample that test requires. Your provider may also test you for chlamydia. These infections often occur together.
Management and Treatment
How is gonorrhea treated?
You'll need antibiotics to treat gonorrhea. Your partner(s) will need treatment, too. The CDC currently recommends a shot of Ceftriaxone, with dosage based on your weight:
- 500 milligrams of Ceftriaxone if you weigh less than 150 kilograms (about 330 pounds).
- 1 gram of Ceftriaxone if you weigh more than 150 kilograms.
If you're allergic to Cetriaxone, your healthcare provider may give you a shot of Gentamicin (240 milligrams) plus 2 grams of Azithromycin. You'll take Azithromycin by mouth (orally).
Your provider may prescribe additional medication, like doxycycline, to clear a co-infection with chlamydia. Follow your provider's instructions on what medications to take and when.
It's important to consider what treatment can and can't do. Treatment can rid your body of the bacteria. Treatment can't:
- Undo any damage to your body that the infection may have caused before treatment.
- Protect you from future gonorrhea infections.
It's important to take preventive steps to protect yourself after treatment so that you don't get re-infected.
Can gonorrhea be cured?
Yes. Prompt treatment can cure gonorrhea. Take all medicine as your healthcare provider instructs, even if your symptoms improve and you start to feel better. Also, never take someone else's medicine to treat your illness. Doing so makes the infection harder to treat.
Taking all antibiotics as prescribed is always important, but it's especially important with gonorrhea. Gonorrhea is curable now, but it's becoming more resistant to antibiotics. Some forms of gonorrhea that have developed a high level of antibiotic resistance are commonly referred to as "super gonorrhea."
To ensure that gonorrhea remains curable, it's more important than ever that everyone take medications as prescribed – and that everyone takes steps to prevent infection.
Prevention
How can I prevent gonorrhea?
The only way to prevent gonorrhea is not to have sex. For many people, a more realistic goal is to reduce the risk of contracting and spreading gonorrhea. Take these steps to reduce your risk:
- Always use a condom or dental dam during sex.
- Don't have sex with someone who has an active infection.
- Don't have sex with someone who has gonorrhea symptoms.
- Limit sexual partners and communicate openly about sexual activities.
- Get tested for gonorrhea and have your partners get tested, too.
There's no perfect protection for gonorrhea if you're sexually active. For instance, condoms can tear. Still, taking extra precautions during sex can greatly reduce your risk of infection.
How often should I get tested for gonorrhea?
The CDC recommends that all people assigned female at birth who are sexually active and under 25 get tested for gonorrhea each year. Regardless of sex, you may need to get tested annually if you're considered high risk for contracting gonorrhea. Your risk factors include your age and sexual activity. Factors like how common gonorrhea is in the area you live in are also important.
Talk to your healthcare provider about how often you should get tested based on your risk.
Outlook / Prognosis
What is the outlook for people with gonorrhea?
People who get prompt treatment and follow treatment instructions carefully can resume their normal lives. Untreated gonorrhea can cause several long-term health problems. Gonorrhea can even be life-threatening without proper care.
Complications in women
In people assigned female at birth, untreated gonorrhea can:
- Spread to other reproductive organs, including your uterus and fallopian tubes, and cause pelvic inflammatory disease. PID can cause infertility and ectopic pregnancies, which can be life-threatening to the mother (birthing parent) and the baby.
- Cause eye problems in infants born to untreated birthing parents, leading to blindness.
- Spread to other body parts, causing swollen and painful joints, liver inflammation, and heart valve and brain damage.
Complications in men
In people assigned male at birth, untreated gonorrhea can cause:
- Infertility.
- Scars in the urethra.
- Inflammation of the testicles.
- Prostate pain and inflammation.
- Other problems if it spreads throughout the body, including swollen and painful joints, liver inflammation, and heart valve and brain damage.
What happens if I get gonorrhea during pregnancy?
Talk to your healthcare provider. You can pass the infection on to your baby during delivery, which can cause health problems for your newborn. Babies born to birthing parents with untreated gonorrhea are at risk for complications like low birth weight and blindness.
Your provider will help you get the right testing and treatment to keep you and your baby safe.
Living With
Can I have sex after gonorrhea treatment?
Your healthcare provider will give you instructions about when you can resume sex. Typically, you need to wait at least a week after you and your partner(s) finish all your medications before having sex. Wait until your symptoms have gone, too.
How can I take care of myself?
If you are sexually active and considered high risk for gonorrhea, consider regular STI testing. Since many STIs, including gonorrhea, don't cause symptoms, you could have an infection and pass it onto others without knowing it. Untreated gonorrhea can also cause complications that you can avoid with regular testing and prompt treatment.
What questions should I ask my healthcare provider?
If you have gonorrhea, questions you may ask include:
- What tests will be needed to diagnose gonorrhea?
- Would you recommend testing for chlamydia also?
- How will I know if the infection has damaged my reproductive tract?
- How can I be sure that the medication cleared my infection?
- How should I inform my partner(s) that they may have gonorrhea?
- How do I know how long I may have been contagious (and passing the infection to others)?
- How can I avoid re-infection while still enjoying a healthy sex life?
Frequently Asked Questions
What happens if you have gonorrhea?
Begin antibiotic treatment as soon as possible. Alert your partner(s) so that they can get tested and treated, too. You may need to abstain from sex while the medicine fights the infection, but currently, antibiotics can cure gonorrhea.
Does gonorrhea have a smell?
A foul-smelling discharge isn't a common symptom of gonorrhea. A smelly vaginal discharge – especially a fishy smell – may signify a vaginal infection unrelated to gonorrhea. Schedule an appointment with your provider if you notice an unusual smell and are worried about your health.
Which is worse – chlamydia or gonorrhea?
Both gonorrhea and chlamydia are highly contagious and can cause long-term damage to your health without treatment. You should avoid both infections as much as possible by practicing safer sex. Get treated immediately if you learn that you or your partner is infected.
A note from Cleveland Clinic
The best way to avoid gonorrhea is to use a condom or dental dam during any sexual activity. Safer sex is especially important with gonorrhea since it often doesn't cause symptoms. If there's a chance you've been exposed, don't let embarrassment prevent you from scheduling a visit with your healthcare provider. Get tested immediately. Untreated gonorrhea can cause long-term damage to your health. You shouldn't have to experience these complications, especially when a simple course of antibiotics can cure your infection.
Comments
Post a Comment